Judy, Labels, and What Service Dogs Actually Do
Reviewing health notes after a recent routine doctor’s appointment, something small—but significant—came up. I noticed that my doctor documented that Judy was with me but not helping with mobility during the visit. That moment gave me pause—not because it was wrong, but because of how easy it is for service dogs to be misunderstood.
To be clear, for this visit, we had literally walked about ten steps into the exam room and sat down in a chair. Judy remained “under” the chair for the duration of the 20-minute visit. That was it. No doors to open and no mobility support needed. Judy was working, just quietly—like she so often does.
It reminded me that many people (even well-intentioned professionals) aren’t always familiar with how service dog training categories work, or how complex real-world disability support can be. So for my curious friends and readers, here’s a little more context.
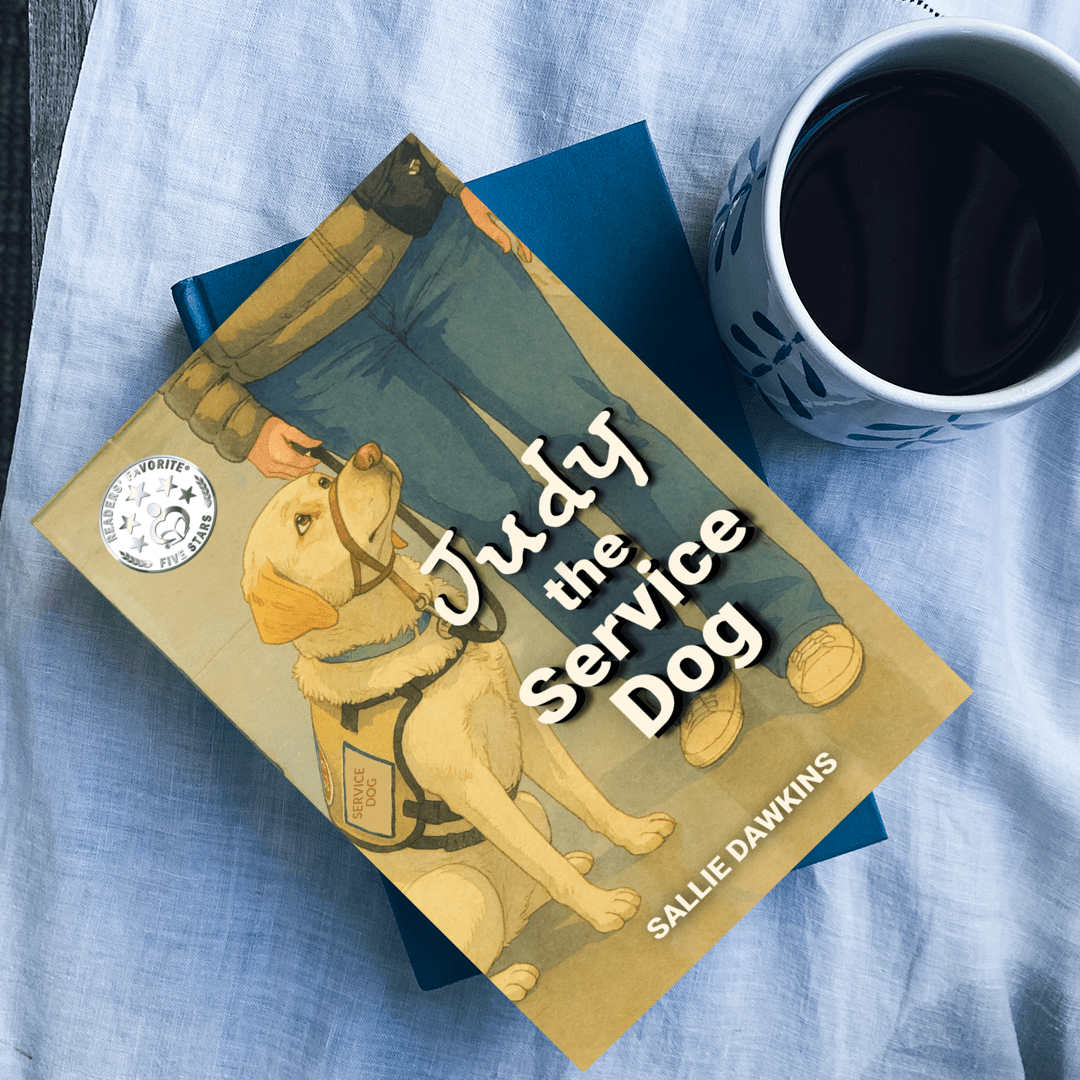

Judy the Service Dog (Yes, That Judy)
If you’ve read Judy the Service Dog, you already know that Judy didn’t just wake up one day knowing how to help me.
Judy was trained through America’s Vet Dogs, an Assistance Dogs International (ADI)–accredited program. That means she completed extensive, standardized training and testing before being placed with me. Her certification is PTSD Mobility Service Dog, which sometimes raises eyebrows. People assume that label means she must be physically supporting me every moment she’s working.
That’s not how it works.
What Judy Is Trained to Do
Like all professionally trained service dogs, Judy mastered Obedience & Control and Public Access Skills—the foundation that allows her to work calmly and safely anywhere the public is allowed.
Obedience & Control skills include:
- Sit
- Down
- Stay
- Heel (loose-leash walking on left side)
- Side (walking on right side)
- Come
- Place / Mat
- Leave it
- Drop it
- Under (tuck neatly under tables/chairs)
Public Access Skills include:
- Ignoring food, people, animals
- Calm behavior in crowds
- Riding elevators, public transit
- Remaining settled for long periods
- No barking, lunging, or soliciting attention
Beyond that, Judy’s PTSD Mobility-specific tasks include:
- Interruption during escalating anxiety or dissociation with gentle nudges
- Deep Pressure Therapy (DPT) or grounding through physical contact to help re-regulate my nervous system
- Cover or “Center” to create space in crowded environments
- “Turn” (to let me know what’s going on behind me)
Just as important—though less obvious—is her presence. Judy’s calm, predictable behavior is deeply affirming. Her established routines for sleeping, waking, eating, and taking breaks played a crucial role in helping me recover from months of nervous system imbalance that had thrown my circadian rhythm into disarray.
When the Nervous System Goes Offline
Part of my health picture includes chronic pain from Ehlers Danlos Syndrome (EDS). With EDS, joint hypermobility and instability often result in frequent dislocations and subluxations, causing significant discomfort. Muscular compensations and overuse of surrounding tissues can lead to myofascial pain, while nerve compression and neuropathic pain further compound the problem.
Many individuals suffer from symptoms resembling Long-COVID, which may include diagnoses such as Ehlers-Danlos Syndrome (EDS) or hypermobile EDS, Postural Orthostatic Tachycardia Syndrome (POTS), and Mast Cell Activation Syndrome (MCAS). In the case of POTS, autonomic dysfunction can lead to a rapid heartbeat, dizziness upon standing, sleep disturbances, anxiety, brain fog, and challenges in regulating body temperature. MCAS can have widespread effects on various bodily systems, including neurological, cardiovascular, gastrointestinal, and musculoskeletal. Common symptoms of MCAS include allergic reactions such as urticaria or anaphylaxis, flushing and sweating, gastrointestinal issues, breathing difficulties, muscle atrophy, and chronic fatigue.
At times of intense stress, multi-system dysregulation and dysautonomia would cause my nervous system to essentially short-circuit, leading my brain to shut down. It became extremely challenging to think clearly, process information, or manage my emotions, which intensified my perpetual state of fight-or-flight. Conditions like ADHD, ASD, anxiety, and depression aren’t isolated issues; rather, they are natural responses. The support I’ve received from Judy, including her task work, routines, and grounding techniques, has been essential in helping my nervous system learn that it’s safe.


Mobility Support Isn’t All-or-Nothing
Judy is also trained in light mobility support, which comes into play when it’s needed.
She indirectly supports issues related to Ehlers-Danlos syndrome (EDS), including pain, fatigue, and occasional gait disturbances. Judy helps with forward momentum (which is phenomenal when we’re taking walks); balance support in transitional movements; and she encourages pacing through regular walks and play (yes, playing ball counts as therapy). Those breaks help manage chronic fatigue and reinforce healthy movement patterns—something my body doesn’t always self-regulate well.
About Disclosure (or the Lack Thereof)
Under the Americans with Disabilities Act (ADA), I’m not required to disclose diagnoses, training details, or task lists to anyone. Not doctors. Not strangers. Not curious bystanders.
Still, people ask because they care—and because service dogs are still widely misunderstood. I'm sharing this not to justify their presence, but to provide insight into the vital roles service dogs like Judy play. Often, their most significant contributions occur in silence. At times, the dog may simply be "there," yet that presence alone can be what keeps everything else running smoothly.
I appreciate your curiosity, kindness, and openness to learning with me. Judy would approve—after her next scheduled nap, of course.

.png)